DNR ORDERS CAN LEAD TO WORSE CARE & INCREASE DEATH RATES
Posted: Aug 20th, 2021 at 05:05PM
While do-not-resuscitate (DNR) orders have been a prominent part of the medical landscape for decades, misconceptions persist among patients, their families, and even healthcare providers about what such orders mean.
And an increasing body of medical literature suggests that patients and their families may want to take a moment to consider all options and do additional research before agreeing to sign a DNR. That’s because multiple studies have connected the presence of DNR orders to elevated death rates, poorer medical care, and negative health outcomes.
This e7health.com analysis of 10 peer-reviewed studies indicates that while it can reduce needless suffering, which was the original intent of DNR orders, DNR often has become a self-fulfilling prophecy. If it were a medication, it would be pulled off the market because of its sometimes unintended consequences.
Let’s take a look at what the medical literature says and explore other facets of DNR you may not know about.
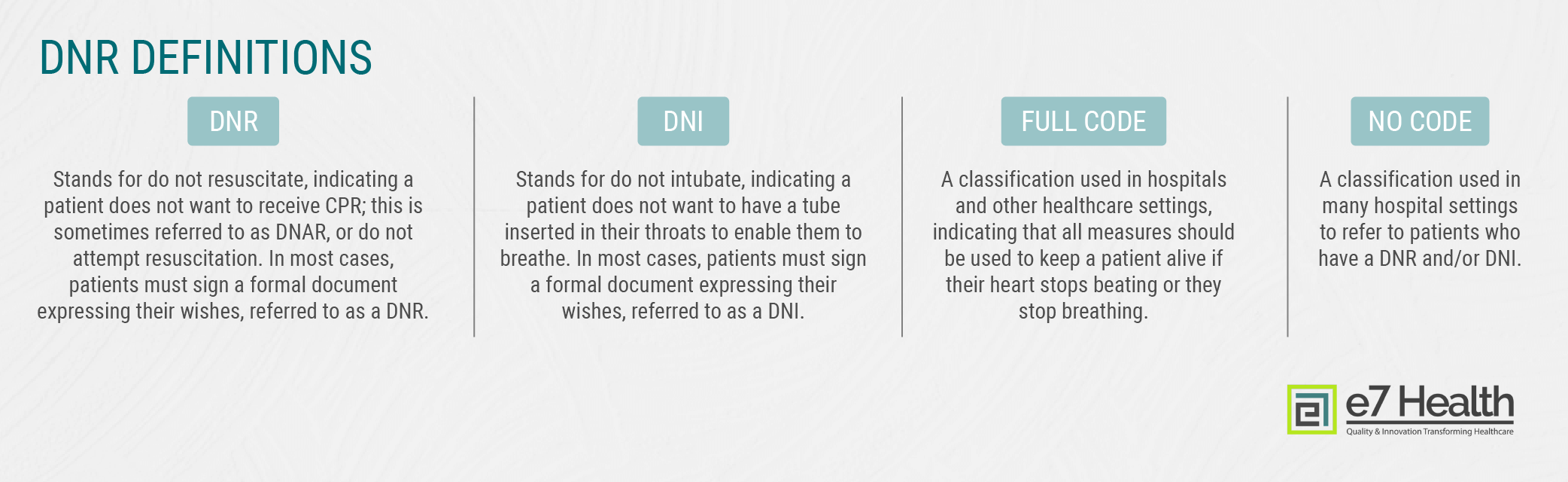
Definitions: What Is DNR?
Before we share the scary statistics surrounding poor health outcomes related to DNR orders, it’s helpful to understand some of the terminology surrounding this issue. It’s also important to note that while these definitions apply generally, individual healthcare facilities and even individual providers may use different terminology. It’s best to over-communicate with your healthcare providers with regard to the DNR topic.
MEDICAL research INCREASINGLY CONNECTS DNR ORDERS WITH HIGHER DEATH RATES
While having a DNR or DNI order may not adversely affect you or your loved one, multiple studies have indicated that all other factors being equal, patients with DNR's have higher death rates unrelated to a medical issue that was used to make the DNR decision.
Put another way: A person with a DNR or DNI is more likely to be someone who is nearing the end of their life and may be suffering from a serious illness. But some studies have indicated that the presence of the DNR or DNI itself increases death rates, unrelated to a disease or trauma.
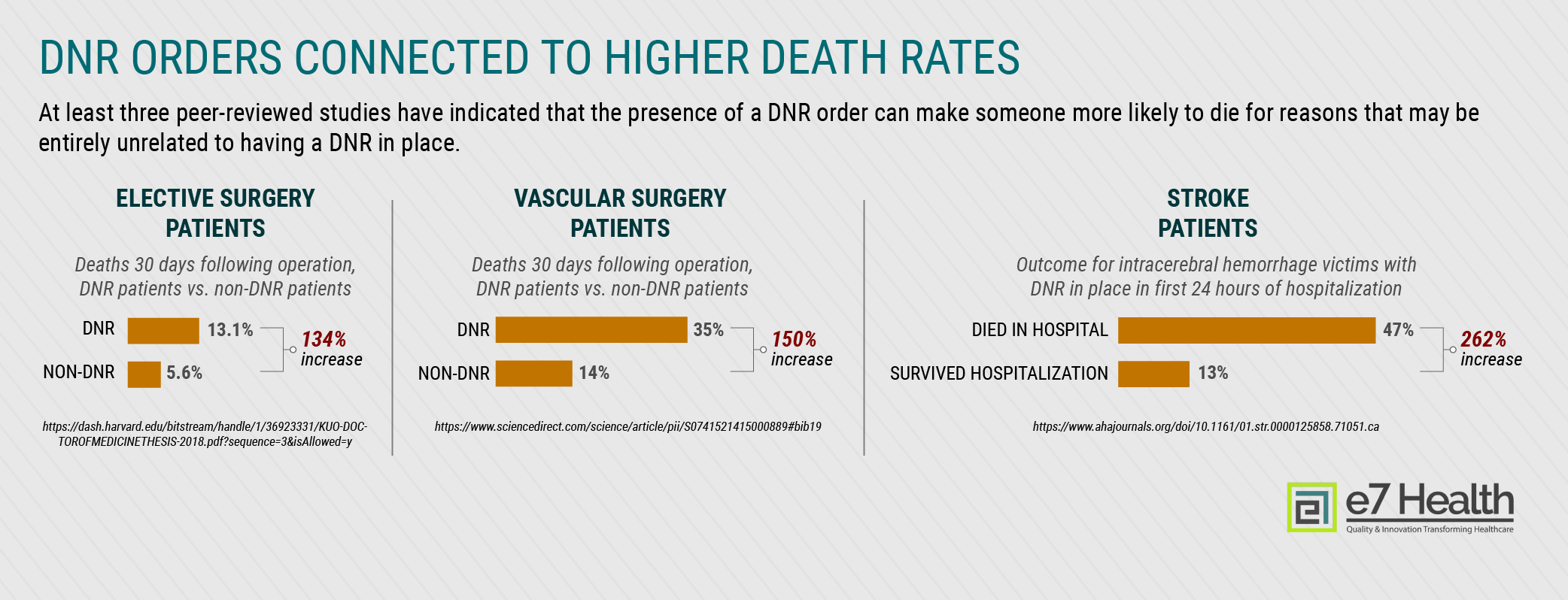
The statistics here are quite disturbing:
- DNR doubled the death rate for surgical patients: A Harvard Medical School study of patients undergoing elective procedures found that the presence of a DNR increased death rates despite no difference in disease rates. [1] About 13 percent of patients with DNR orders in place died within the first 30 days after surgery compared to just under 6 percent for those without DNR orders, while DNR patients who survived had lower rates of most postoperative complications, including pneumonia, surgical site infection, and kidney failure.
- Death rates increased by 150 percent for DNR patients who had emergency vascular surgery: Those who had a DNR in place were more likely to experience graft failure (about nine percent vs. about two percent), while 35 percent died within 30 days of surgery compared to 14 percent without a DNR. [2]
- Almost half of stroke victims who were designated DNR within the first 24 hours died in the hospital: A California study of people who had intracerebral hemorrhage, a severe type of stroke, found that 47 percent of patients who had a DNR within the first day of admission died in the hospital, while only 13 percent survived hospitalization. [3]
DNR Does Not Mean Do Not Treat, But That’s What Happens in Many Hospitals
The presence of a DNR does not indicate the patient would rather end their lives. Rather, a DNR or DNI order means simply that the person does not wish to be revived and have their lives extended through heroic measures. But in many hospitals, DNR may as well stand for DNT (do not treat).
A study on how medical professionals perceive cancer patients with DNR orders indicated that 11 percent of nurses and doctors agreed that DNR was synonymous with “comfort measures.” [4]
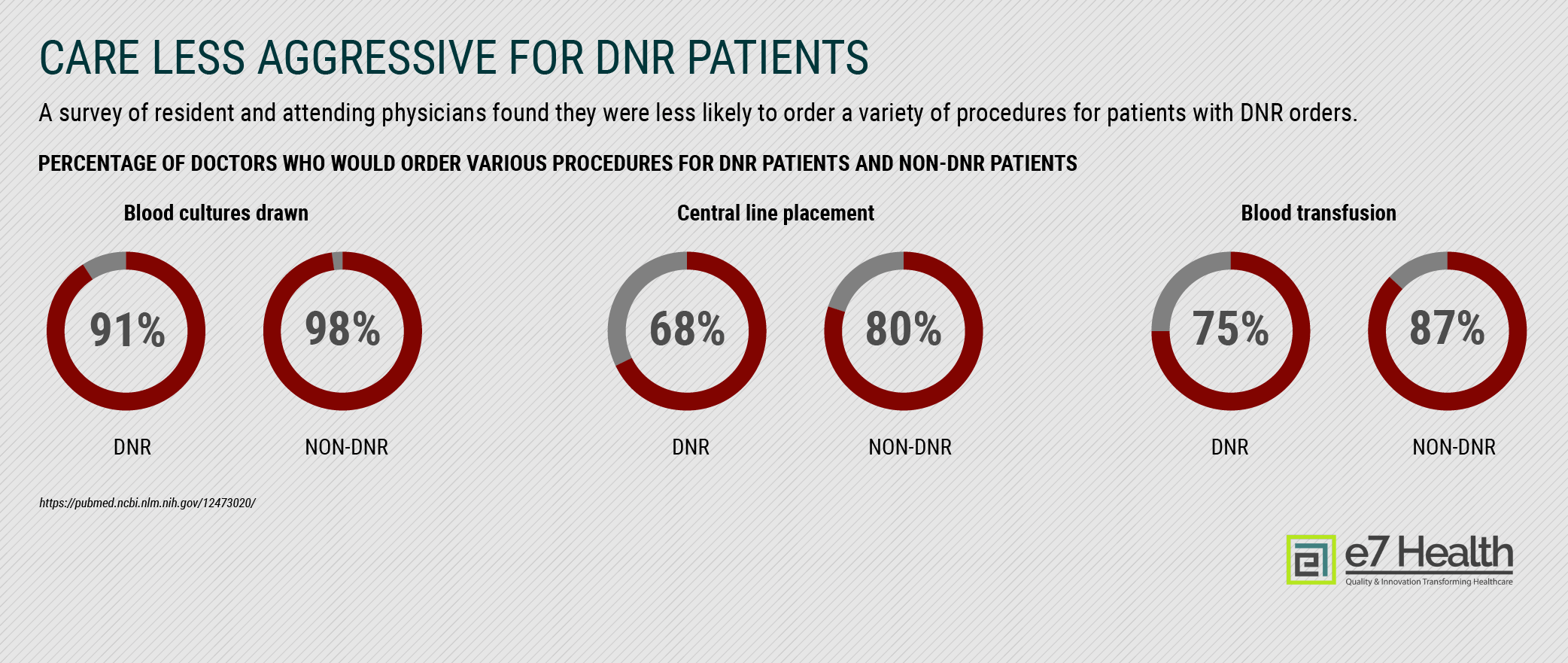
A separate study on care received by geriatric patients found that the presence of a DNR order was associated with patients receiving less care overall, even when that care was not related to heroic measures or resuscitation. Patients with DNR orders were seven percentage points less likely to have blood cultures drawn, 12 percentage points less likely to have a central IV line placed, and 12 percentage points less likely to receive a blood transfusion. [5]
Finally, a study on internal medicine residents found that resident physicians were less likely to provide aggressive treatment to DNR patients like dialysis, surgical consultation, or transfer to intensive care despite not having specific guidance from patients or their family members. [6]
Rules Are More Complex Than Just Not Providing CPR
From a literal standpoint, DNR orders apply only to cardiopulmonary resuscitation, also known as CPR. But this isn’t the only form of attempting to revive a person whose body is failing in some way. CPR involves chest compression or stimulation, but many people may consider a do-not-intubate order, or DNI, which means they do not want a breathing tube placed in their throats.
In hospitals, this is typically referred to as code status, and in the absence of advance directives, it’s typical for all patients to receive “full-code” status, meaning that if their hearts or breathing stopped, all possible measures would be taken to save their lives.
DNR's Aren’t Just for Elderly People
The presence of advance directives varies widely, and those who are nearing the end of their lives, whether because of age or disease, are the most likely to have DNR or other orders in place.
A CDC report found that an estimated 17 percent of home healthcare patients under 65 had advance directives compared to 41 percent of those over age 85. [7] Home healthcare patients may receive medical care that includes medication dispensing or checking of vital signs, but they are not necessarily critically ill patients.
But those who have been discharged from hospice care are those most likely to be nearing the end of their lives, and age-based differences were considerably less dramatic among this group. More than nine in 10 discharged hospice patients over 85 had advance directives, while this figure was 81 percent for those under 65.
Making a Decision in the Early Stages of a Crisis Can Be Deadly
 In an emergency situation, every moment counts, and it’s understandable for medical professionals to urge individuals and their loved ones to determine the best course of care in a timely manner. But that does not mean that patients and their families should be rushed into making decisions about DNR/DNI orders.
In an emergency situation, every moment counts, and it’s understandable for medical professionals to urge individuals and their loved ones to determine the best course of care in a timely manner. But that does not mean that patients and their families should be rushed into making decisions about DNR/DNI orders.
Studies have suggested that doing so can have deadly consequences that may have been avoidable.
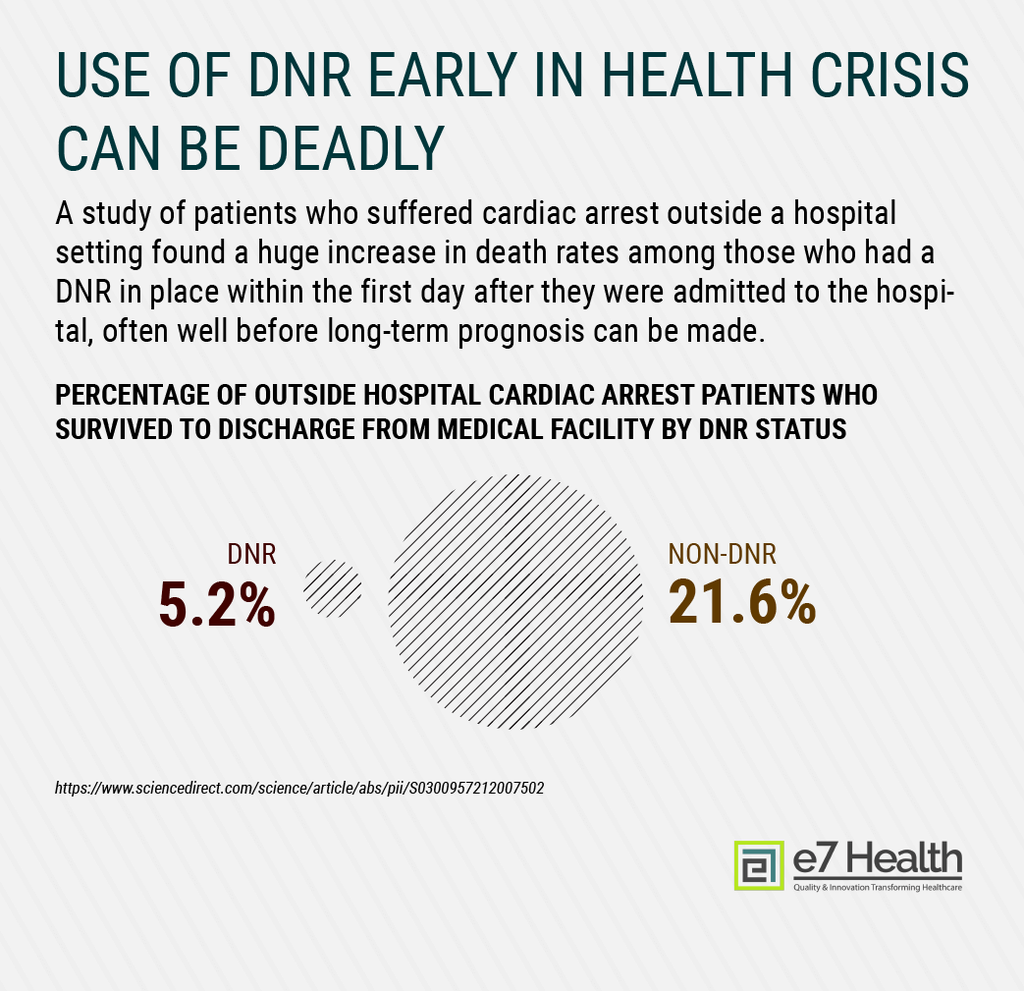
In addition to the California stroke study referenced earlier, which found that a DNR signed within 24 hours of a person having a stroke more than tripled the patient’s risk of dying in the hospital, a separate California study of cardiac arrest patients found that only five percent of those who had a DNR issued within the first 24 hours after hospital admission made it out of the hospital compared to about 22 percent of those with no DNR. [8]
Healthcare Facilities and Individual Professionals Handle Orders Differently
No single national DNR standard exists for healthcare providers, and this variation means that even within the same city, patients at different hospitals can receive wildly different care.
The California DNR stroke study referenced earlier also sought to quantify the differences in how hospitals and medical facilities handle DNR patients. Researchers found that DNR rates, meaning the percentage of patients with such orders, varied between zero and 70 percent and that services received in hospitals that use DNR orders 10 percent more frequently than similar facilities resulted in a 13 percent increase in the odds that the patient would die. [9]
DNR Laws Vary by State & No Single Legal Standard Applies Across the Board
Just as no single medical standard exists when it comes to advance directives like DNR or DNI orders, there is no one legal standard that applies across the country, either. While most states have laws on the books, orders may not be honored between states, and other differences can make it difficult to ensure that the patient’s wishes are followed.
For example, in Virginia a DNR order cannot be suspended temporarily, such as for the person to undergo a needed surgery. Instead, the patient must revoke their existing DNR and write a new one, but patients may not be aware of this and may not have both orders. [10] And in Florida, a DNR must be printed on yellow paper to be considered legally valid. [11]
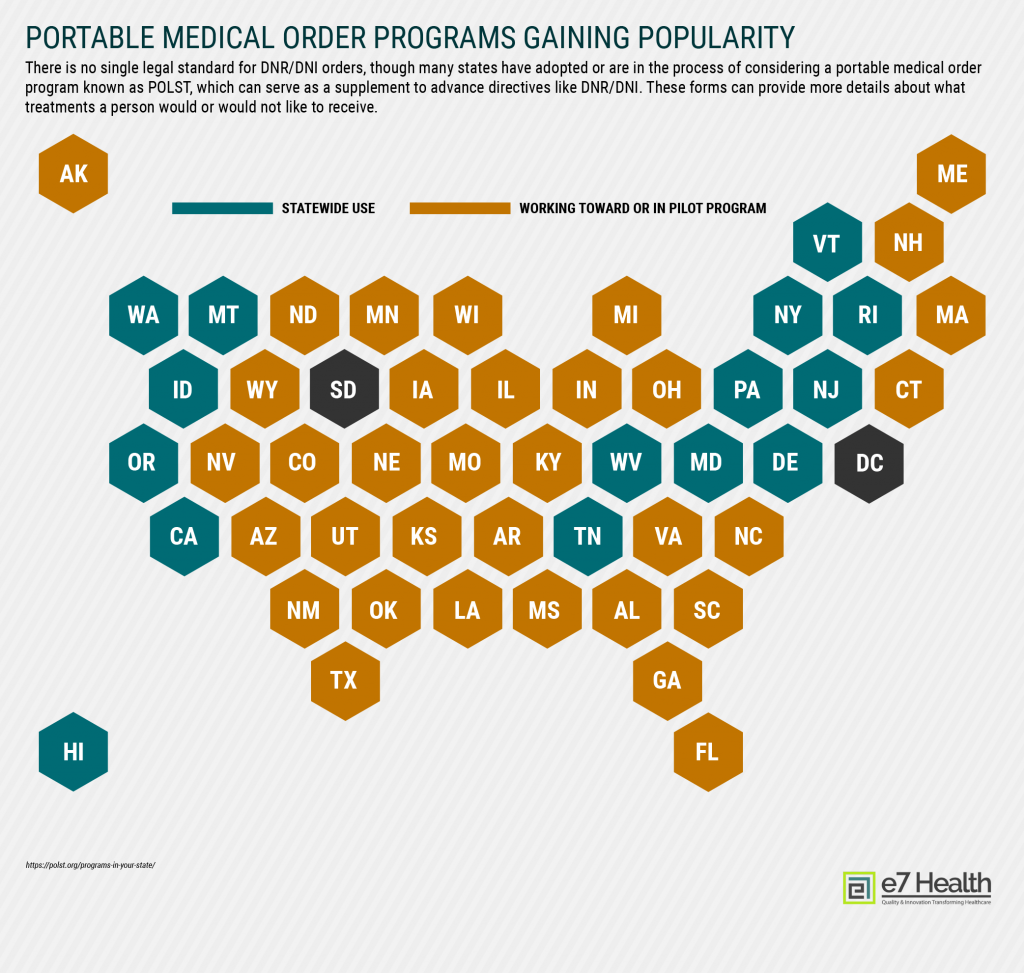
While not DNR/DNI guidance, many states have launched POLST (portable medical order) programs, which aim to help patients provide more details about what treatments they would or would not like to receive. Six states have adopted the form, which is meant to supplement advance directives like DNR/DNI, while dozens more are considering them or working to adopt them. [12]
Conclusion
Every person wants and deserves to have their medical wishes honored, especially when it comes to experiencing a traumatic and potentially painful medical intervention like CPR or intubation. While the presence of DNR and DNI orders have helped many people make their own medical decisions, the reality is not black and white. At a minimum, individuals and their loved ones should have thorough discussions with themselves and their medical care providers about exactly what might happen if they sign a DNR or DNI.
References
[1] https://dash.harvard.edu/bitstream/handle/1/36923331/KUO-DOCTOROFMEDICINETHESIS-2018.pdf
[2] https://www.sciencedirect.com/science/article/pii/S0741521415000889#bib19
[2] https://www.ahajournals.org/doi/10.1161/01.str.0000125858.71051.ca
[4] https://ascopubs.org/doi/abs/10.1200/jco.2010.28.15_suppl.9078
[5] https://pubmed.ncbi.nlm.nih.gov/12473020/
[6] https://pubmed.ncbi.nlm.nih.gov/28099054/
[7] https://www.cdc.gov/nchs/products/databriefs/db54.htm
[8] https://www.sciencedirect.com/science/article/abs/pii/S0300957212007502
[9] https://www.ahajournals.org/doi/10.1161/01.str.0000125858.71051.ca
[10] https://forum.ashrm.org/2018/05/23/is-universal-national-dnr-possible/
[11] https://www.nolo.com/legal-encyclopedia/do-not-resuscitate-orders.html